Since it was enacted in 1965, Medicaid has been helping low-income individuals receive proper medical care they usually couldn’t afford.
As part of the program, non-emergency medical transportation (NEMT) providers help patients get to their appointments, especially if they don’t have a vehicle or have a disability.
While NEMT businesses provide an incredible service to Medicaid recipients, getting paid for these trips can be more challenging than they might expect.
In this article, we highlight some of the most significant Medicaid billing challenges NEMT providers need to be aware of and offer suggestions on overcoming these obstacles—or even avoiding them altogether.
Complex Medicaid Regulations and Rates
As the program has evolved over the decades, the Medicaid system has become more involved.
The same is accurate for rates and regulations involving NEMT transportation. There are numerous steps providers must take to ensure they comply with the mandates of their state Medicaid program. Reimbursement rates and how reimbursements for trips are handled can change as well.
All these fluctuations can make it more difficult for providers to maintain a financially viable business model.
To stay aligned with any changes or updates to Medicaid’s NEMT rates and regulations, providers need to consistently keep up with news and updates in their state and region.
Business owners should maintain close relationships with their state and regional brokers, managed care organizations (MCOs), or the state’s in-house Medicaid transportation management to do this effectively. Consistent communication with these contacts makes understanding any rate or regulation changes easier.
It also helps to have someone in these organizations to answer questions on claims or reimbursement issues.
Do More with Less
Handle more trips with fewer dispatchers on your payroll with Tobi.
Start for FreeComplications in the Claim Process
While NEMT is designed to make it easier for patients to get to appointments, it’s much more challenging for providers to get reimbursed for these trips.
From patient eligibility to filing to delays, there are multiple ways for payments to get held up in the Medicaid system.
Verifying Patient Eligibility
Medicaid won’t reimburse providers for trips if the patients they transport aren’t beneficiaries.
Confirming that your customers are eligible and registered under Medicaid is critical before providing service.
Any claim filed for that trip will be denied if they aren’t eligible, and providers will lose revenue.
Incomplete Documentation
After a trip, NEMT operators must send an attestation request to brokers or MCOs for approval. From there, the claim for transportation can be submitted to Medicaid.
If there’s an issue with the attestation process, it won’t be approved, and reimbursement claims can’t be submitted.
If attestation is approved and everything is submitted to Medicaid, accurate documentation of services is necessary for successful billing. Incomplete or inaccurate records can lead to claim denials and delays in payment.
Errors in billing codes, modifiers, or other details can also lead to claim rejections. Identifying and rectifying these errors promptly is crucial for successful reimbursement.
Submitting Claims on Time
Even if claims have all the necessary information completed, more issues arise if they aren’t sent on time.
Medicaid programs often have strict deadlines for how soon a claim must be submitted after service. If these deadlines aren’t met, it can lead to reduced reimbursement or even the denial of a claim.
Payment Delays
Ensuring every claim is submitted correctly and on time is crucial but doesn’t guarantee reimbursements are paid out quickly.
Even if providers do everything right, the Medicaid reimbursement process can be slow, delaying critical cash flow.
While Medicaid recipients tend to be a majority of customers for NEMT providers, expanding their businesses to adopt more private pay clients can help supplement income, especially when the reimbursement process takes longer than expected.
NEMT Software as a Solution
While many of these challenges can be solved in other practical ways, one of the most straightforward solutions to these obstacles is finding the right NEMT software to help run your operation more effectively and efficiently.
With the right solution, providers can more easily keep track of all the vital information necessary to expedite Medicaid claim submissions and reduce the likelihood of manual errors.
At Tobi, we provide a complete NEMT software solution that addresses common challenges:
Complex Regulations and Rates: Tobi was built to adhere to NEMT rules while effectively meeting federal and state compliance requirements.
Verifying Patient Eligibility: Tobi’s system tracks which provider each booking comes from (e.g., private pay, broker, etc.), ensuring NEMT operators don’t submit reimbursement claims to Medicaid if a Medicaid provider does not facilitate the patients.
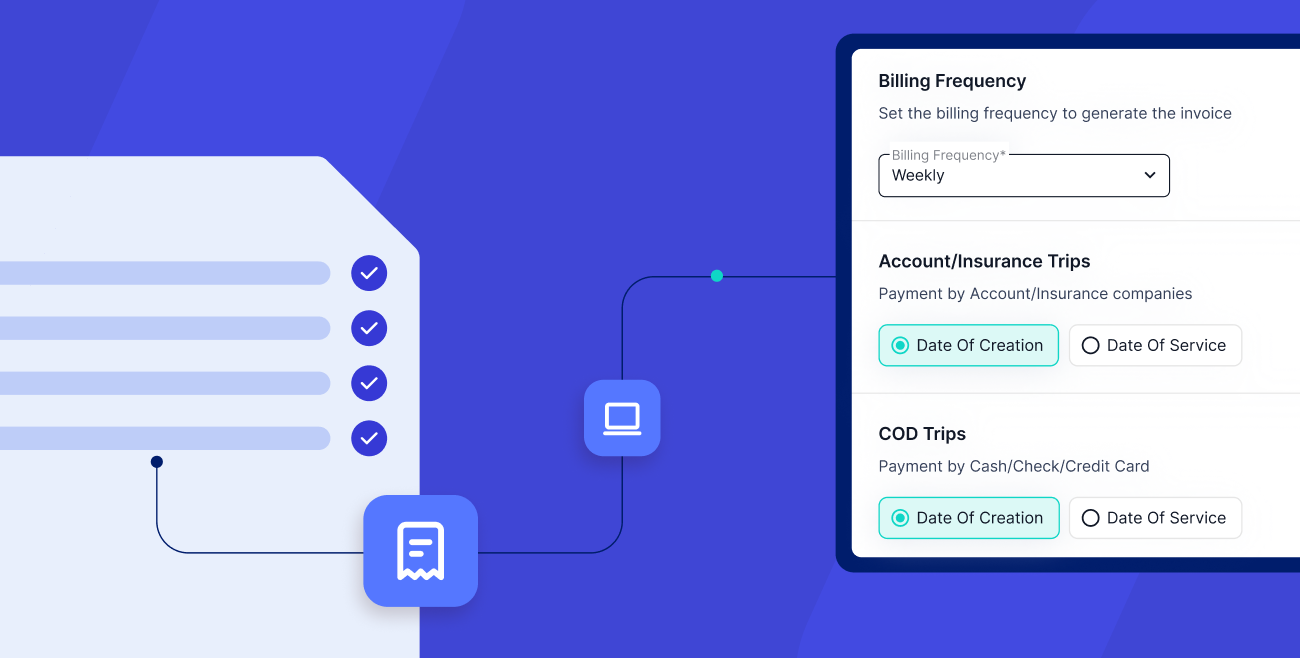
Incomplete Documentation: Tobi submits attestations electronically to verify bookings and get broker approval automatically without extra effort. It easily integrates with third-party billing systems to process attestations and claims within the Tobi platform.
Submitting Claims on Time: With Tobi, you can seamlessly submit and monitor claim statuses through popular applications like Kinetik and Transit Billing and choose between manual or automatic submissions—reducing the chances of late submissions.
Payment Delays: While Tobi can’t make Medicaid move faster, it does track and include all necessary information to ensure claims are approved while sending them automatically so that no delay is caused by missing or inaccurate information by the provider.
Designed By and Built for NEMT Providers
Tobi’s team understands the complexities of the Medicaid industry, designing our product to be the only software solution you need.
Tobi makes compliance simple by tracking, recording, and verifying service delivery electronically with GPS data. Not only can you streamline driver workflows and records management, but you can even manage e-attestation and claims more accurately.
With Tobi, the guesswork of getting paid is eliminated, letting you track and resolve all invoice and claim issues in one place. You can remove human error and handle claims quickly and efficiently with any billing platform.
Are you curious to see how Tobi can help you run your NEMT operations more efficiently? Request a demo for a free 30-day trial and experience how Tobi makes your business better at every turn.